- What We Do
- Back
- Enterprise Solutions
- Revenue Recovery
- Revenue Optimization
- Clinical Integrity
- Regulatory Navigation
- Who We Help
- Our Platform
- Insights and Resources
- About Us
- Careers
- Our Platform
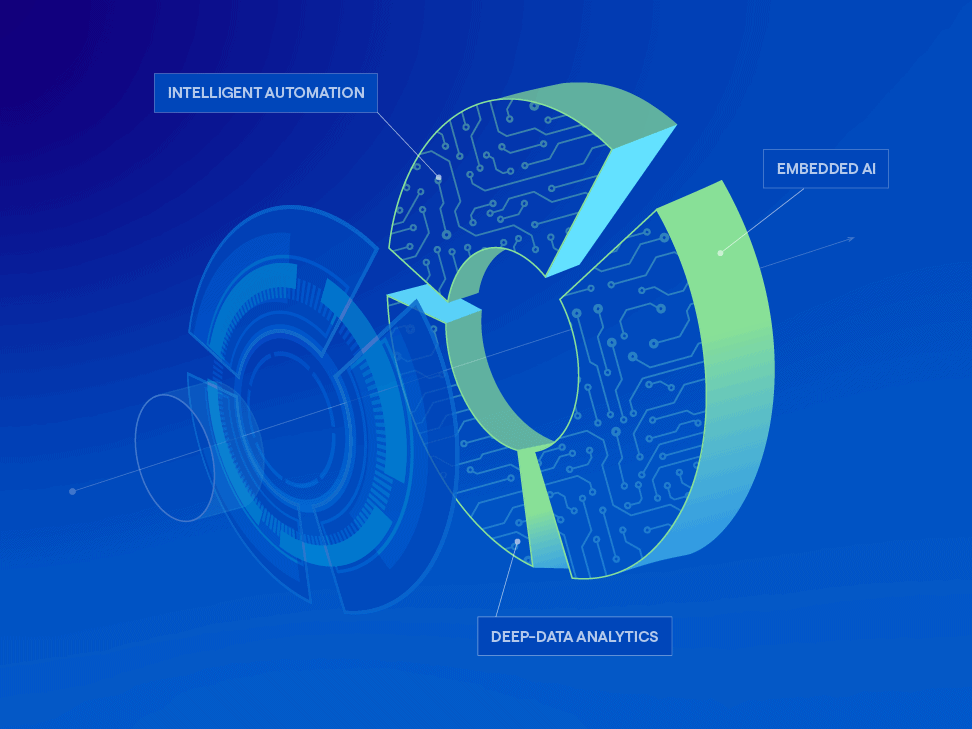
A platform powered by intelligent tech and next-level expertise
Reimagine the revenue cycle with a future-ready platform
The R1 Platform brings the power of AI, Intelligent Automation and Deep Data Analytics to healthcare through proprietary RCM optimization engines that turn complex data into financial and operating performance improvements – enabling leading healthcare organizations to deliver outstanding patient care today and in the future – with confidence
Where deep RCM experience meets intelligent technologies
The R1 Platform was purpose-built by seasoned revenue cycle operators to bring the industry’s most intelligent technologies, proprietary RCM optimization engines and advanced analytics to transform the revenue cycle.
With data at the core fueling R1’s AI and automation capabilities, the R1 Platform employs optimization engines to uphold accuracy, efficiency, and compliance across the revenue cycle, enabling our clients to stay at the forefront of a rapidly evolving financial landscape.
R1 Embedded AI uses real-time data and several forms of AI including machine learning, natural-language processing and generative AI, to deliver more automation, increased productivity and greater patient satisfaction.
R1 Intelligent Automation unlocks the equivalent of 5,000 FTEs in operational capacity by automating routine and repetitive activities, optimizing workflows and improving team productivity.
The R1 Platform uses data and analytics to improve reimbursement and drive efficiency, leveraging access to data from over 90 of the top 100 health systems and more than 550M patient records accessed nationally per year.
Encompassing more than 20,000 algorithms derived from our work with 95% of US payers and every major EMR, the R1 Rules Engine enforces and automates complex revenue cycle processes to optimize user workflow and maximize revenue opportunities with accuracy and compliance.
Acting as the revenue cycle’s “central nervous system,” our Workflow Orchestration Engine coordinates and optimizes the myriad of steps required to drive financial outcomes by seamlessly blending automated and human-centric workflows.
R1 Contract Modeling and Pricing validates reimbursement accuracy, simplifies contract management, helps recover underpayments and streamlines workflow to ensure that health plans are complying with their contract terms and are being reimbursed appropriately.
A strategic alliance to propel generative AI for the revenue cycle
LEARN MORER1 and Microsoft joined forces to accelerate the development and integration of generative AI into R1’s industry-leading RCM platform. By combining R1’s deep revenue cycle data and expertise with Microsoft’s AzureAI, R1 clients will realize immediate benefits that benefit providers and the patients they serve.
The platform engineered to optimize your revenue cycle at scale
Efficiency at every step
R1’s Platform is at the forefront of innovation, purposefully integrating data and creating a virtuous feedback loop that optimizes every facet of the revenue cycle.
With each data interaction, our intelligent and proprietary technology, coupled with deep connections, workflow and analytics capabilities, unlocks revenue opportunities efficiently and drives results at scale.
Bridging data in a seamless way
The R1 Platform is a data powerhouse that integrates and unifies millions of clinical, financial and patient datapoints to enable accurate, reliable and secure information exchange, across all data sources.
R1’s Unified Data Exchange is designed to integrate with every major EMR, payer, clearinghouse, bank and other data sources. This fluid transfer of data has hundreds of pre-built connections to integrate with multiple data sources, helping to simplify implementation, uphold data integrity and facilitate a seamless connection to the source of truth.
Data that speaks for itself
Intelligent automation
manual tasks automated
200M+
Proprietary rules
rules and algorithms
20K+
Data scale
NPR claims processing visibility
$900B+
Patient records
records accessed annually
550M+
Unlock insights. Maximize results. Stay ahead.
Processing over 550 million patient records annually, R1 is a data powerhouse leveraging real-time data to optimize every aspect of the revenue cycle. With advanced analytics and predictive capabilities, we deliver instant insights, performance transparency and can forecast trends, empowering providers to maintain a competitive edge.
With R1’s data-driven intelligence, our clients have a strategic advantage to maximize performance and stay one step ahead of the curve.
The auth automation and auth creation technology has dramatically improved the lead time that it takes for all of those administrative processes that need to happen from the point the order is submitted. Our big commitment to this it taking as much time and friction out of the process as we can possibly control.”
Mandie Brzon
Ascension, VP Revenue Cycle
R1 is an excellent partner. I would call them a partner, not a vendor. They have been with us for a long time, and as technology grows, they grow with it. They are into global services and automation, and we really like the automation part.”
Underpayments KLAS Report, August 2023
Manager
Ascension’s aspiration is to deliver a best-in-class consumer experience, and our partnership with R1 is a key component in achieving that goal. We look forward to continuing with R1’s technology platform to enable a seamless consumer journey.”
Eduardo Conrado
Ascension, EVP & Chief Strategy and Innovation Officer
R1’s Platform recovers more revenue than any other RCM partner
At R1, we deliver more savings and recover more revenue than any other RCM company. Our platform runs on deep data, integrated analytics and sophisticated automation, which accompanies decades of expertise to proactively identify problems across your revenue cycle, with comprehensive solutions that drive scalable, sustainable results for you and your patients.
Pure performance, end-to-end
Our platform gives you the power to transform every part of your revenue cycle with user-friendly tools, seamless interoperability and an experienced team.
Expansive data, unmatched results
Our platform, purpose-built by RCM experts, leverages our expansive data access and advanced analytics to drive revenue recovery and accelerate cash flow.
Intelligent technology, durable results
We integrate the latest technologies into a single, powerful platform that drives efficiency from patient access to claims and reimbursement.
Deep expertise, comprehensive solutions
Our highly skilled team of deep domain experts leverage technology and deliver comprehensive solutions that meet your needs.
Looking to learn more about us? It all starts here.
The latest from R1
EXPLORE ALL INSIGHTSPrivacy OverviewThis website uses cookies so that we can provide you with the best user experience possible. Cookie information is stored in your browser and performs functions such as recognising you when you return to our website and helping our team to understand which sections of the website you find most interesting and useful.
Strictly Necessary CookiesStrictly Necessary Cookie should be enabled at all times so that we can save your preferences for cookie settings.
If you disable this cookie, we will not be able to save your preferences. This means that every time you visit this website you will need to enable or disable cookies again.
Performance, Functionality, Tracking, and Social CookiesPerformance Cookies
These cookies allow us to count visits and traffic sources so we can measure and improve the performance of our site. They help us to know which pages are the most and least popular and see how visitors move around the site. All information these cookies collect is aggregated and therefore anonymous. If you do not allow these cookies we will not know when you have visited our site and will not be able to monitor its performance.
Functionality Cookies
These cookies enable the website to provide enhanced functionality and personalization. They may be set by us or by third party providers whose services we have added to our pages. If you do not allow these cookies, then some or all of these services may not function properly.
Tracking Cookies
These cookies may be set through our site by our advertising partners. They may be used by those companies to build a profile of your interests and show you relevant adverts on other sites. They do not store directly personal information but are based on uniquely identifying your browser and internet device. If you do not allow these cookies, you will experience less targeted advertising.
Social Media Cookies
These cookies are set by a range of social media services that we have added to the site to enable you to share our content with your friends and networks. They are capable of tracking your browser across other sites and building up a profile of your interests. This may impact the content and messages you see on other websites you visit. If you do not allow these cookies you may not be able to use or see these sharing tools.
Please enable Strictly Necessary Cookies first so that we can save your preferences!